BIOE Faculty Member Develops Low-Cost Cervical Pre-Cancer Treatment Device for Low and Middle-Income Countries
August 8, 2025
A new study led by Fischell Department of Bioengineering (BIOE) Assistant Professor and Fischell Institute Affiliate Fellow Jenna Mueller introduces low-cost medical devices designed to treat cervical pre-cancer in low- and middle-income countries (LMICs). The research, published in Springer Nature, highlights a promising step forward in expanding access to lifesaving care to prevent cervical cancer.
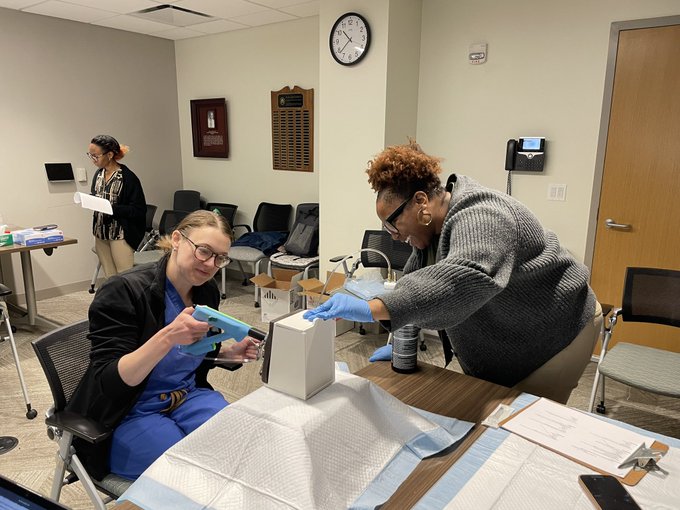
As principal investigator of the Global Biomedical Devices Lab, Mueller and her team evaluated three injector prototypes that deliver a mixture of ethyl cellulose and ethanol (EC-ethanol), a treatment that can be used to safely ablate precancerous cells in the cervix. The study found that one design—an "extender injector"—offered the best combination of precision, ease of use, and affordability. Clinicians overwhelmingly preferred the extender injector, noting its comfort, efficiency, and intuitive design. On average, the device delivered a clinically relevant dose of EC-ethanol in under 20 seconds.
“Cervical cancer causes over 350,000 deaths annually, and 90% of those deaths are in LMICs,” Mueller says. “We believe we can significantly reduce this number in our lifetime if diagnosis and treatment technologies are made accessible to all.”
EC-ethanol therapy builds on earlier work using ethanol ablation in liver tumors. By adding ethyl cellulose, the injectate forms a gel upon contact with tissue, dramatically reducing leakage and off-target damage. The approach enables focused treatment of cervical pre-cancer, the precursor to cervical cancer. By using low-cost tools, each dose of EC-ethanol is expected to cost less than $1, and the preferred injector design can be produced for under $10.
One of the injector designs tested originated from a 2020-2021 BIOE capstone senior design project, which won first place that year. David Garvey, who was a member of the capstone team, was able to continue working on the injector design during his master’s program alongside Fischell Institute Engineer, Kevin Aroom, and Assistant Director, Martha Wang. Garvey’s work was supported by the Fischell Institute's MPowering the State Student Entrepreneurship Fellowship. Garvey is now a Biomedical Engineer at The LaunchPort, a manufacturing and Medtech acceleration center in Baltimore.
The overall EC-ethanol project has been supported by the National Institutes of Health (NIH) Small Business Innovation Research (SBIR) Phase 1 and 2 awards in partnership with Calla Health, a startup focused on accessible cancer technologies.
“This work reflects our commitment to human-centered design,” says Mueller. “We involved providers early in the process and refined the device based on their feedback, which we call the ‘deliver’ phase in design thinking.”
Beyond cervical cancer care, the new injector designs could be applied to other routine gynecological procedures, such as administering paracervical nerve blocks or injecting indocyanine green (ICG) for lymph node mapping.
The team is now preparing for a phase 1 clinical trial at the University of Maryland School of Medicine, where EC-ethanol will be tested in patients scheduled for hysterectomy. Using the Pocket Colposcope, another innovation Mueller has worked on with Calla Health, clinicians will image the cervix and inject EC-ethanol using the extender injector. The excised cervical tissue will then be analyzed to determine optimal dosage. This work will be supported by a multi-million-dollar Method to Extend Research in Time (MERIT) Award (R37), which Mueller recently received from the National Cancer Institute (NCI).
“I am thrilled to receive the R37 award from the NCI,” Mueller says. “It will allow us to test our EC-ethanol procedure in patients and obtain critical safety and early efficacy data needed to clinically translate our technology, bringing us one step closer to reducing cervical cancer deaths in LMICs.”
With the phase 1 clinical trial on the horizon, the research team is focused on gathering the safety and efficacy data needed to move the extender injector toward clinical use. Success in these early stages could pave the way for large-scale implementation in low-resource settings, offering a practical and affordable solution to help reduce preventable cervical cancer deaths worldwide.